Placenta: evaluation
Introduction
- The 'placenta' is strictly defined as the combined maternal and fetal tissues which form an interface between mare and foal.
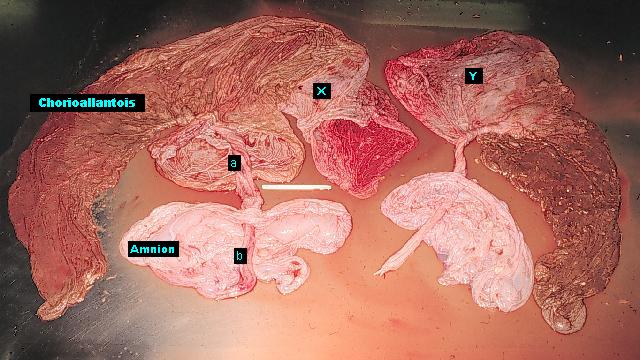
- The tissues which are delivered with the foal at the time of parturition are the 'fetal membranes', these comprise the chorioallantois, the amnion and the placental vasculature (umbilical cord), all derived from embryonic endoderm, mesoderm or ectoderm.
- However, it is common clinical and managerial practice for the fetal membranes to be referred to as the 'placenta'.
- The equine placenta is anatomically defined as diffuse, microcotyledonary and epitheliochorial.
- The placenta's functions include exchange of nutrients and gases, and removal of waste materials.
- Equine placental transfer is inefficient in comparison to other species.
- Poor transfer of nutrients to foal - entire endometrial surface is required for nutrient transfer and gas exchange for one fetus. No placental transfer of large protein molecules, ie immunoglobulins - foal is immunologically naive.
- Transfer of infectious organisms rarely occurs without inducing placentitis and abortion Abortion: overview.
- Endometrial bleeding is possible - blood loss at parturition usually maternal or from premature cord rupture Umbilical cord: premature separation.
- Any factor adversely affecting the intimate relationship of the placenta with the endometrium has the potential to cause serious problems such as abortion, fetal reabsorption Abortion: early embryonic / fetal death, deformity or neonatal infection/compromise Reproduction: prematurity / dysmaturity Foal: neonatal maladjustment syndrome.
- Early placental evaluation provides valuable and potentially life-saving information about the foal Foal: evaluation - neonate and mare and should be performed routinely at all foalings.
Uses
- Examination of the placenta is a vital part of the assessment of the newborn foal and should be carried out within 12 h of parturition. Placental abnormalities may act as indicators for neonatal treatment, eg to prevent sepsis, in advance of clinical signs of illness in the foal.
- Placenta is examined for completeness as soon as possible after foaling as any placental tissue remaining in the mare may be life-threatening Placenta: retained.
- To investigate failed pregnancies and abortions.
- Investigation of status of endometrium which may have implications for subsequent pregnancies.
- Examine the placenta by removing gross debris, laying it on a flat surface and examine each part of the fetal membrane in turn before turning the fetal membranes inside out to examine the opposite surface.
Normal features of the fetal membranes ('placenta')
The skill in examining the placenta is derived from knowing what is 'normal'.- Weight usually c11% of the foal's birth weight.
- Most equine placentas are everted during delivery, ie present with the red, villous surface (the chorion) of the allantochorion showing.
- Check for completeness - the placenta should be a complete mirror image of the uterine body, left and right uterine horns. The parts of the placenta most commonly retained are those equating to the tips of the uterine horns, particularly the non-pregnant horn Placenta: retained.
- The allantoic (foal) side of the allantochorion is usually white and shiny.
- The amnion is the membrane which most closely surrounds the foal. It is white, usually ruptures during foaling, and can be found in the fetal membranes attached about half the way down the length of the umbilical cord. There are often prominent vessels apparent on the surface of the amnion - this is normal.
- The part of the placenta equating to the gravid uterine horn is normally thicker and more edematous than that equating to the non-gravid horn. The umbilical cord is usually c50-70 cm in length with a few twists.
Normal features of the equine fetal membranes ('placenta') which may be confused with pathological features
- ‘Foot pad lesion’: an area of damage to the chorioallantoic membrane caused by pressure from the foal’s foor during late pregnancy.
- Chorioallantoic vesicles: small, focal accumulations of clear fluid within the chorioallantoin.
- Chorioallantoic pouches: the fluid-filled remnants of necrotic, sloughed endometrial cups. Often pedunculated, can be quite big.
- Hippomanes (‘allantoic calculi’): concretions of ions, lipids and cellular debris found within the allantoic cavity; pale brown and liver-like texture; can be quite large, eg 10 cm; historically thought by old fashioned horsemen to be lucky and nailed to the stable wall!
- Congested allantoic capillaries: can be associated with pathology, eg placentitis or amniotic cord torsion, or can be simply areas where blood was compressed in one area of the membranes and pooled elsewhere after expulsion of the membranes.
- Amniotic plaques: focal areas of squamous metaplasia on the amniotic membranes and surface of the umbilical cord.
- The following are areas of the fetal membranes (placenta) which are normally avillous, ie look white rather than red on the chorionic surface of the allantochorion:
- The ‘cervical star’ area, ie where the placenta abuts the cervix.
- The tips of the part of the fetal membranes corresponding to both uterine horns, where the uterine horns abut the oviducts.
- Folds over dominant placental blood vessels.
- The scars corresponding to the position of the (autolyzed) endometrial cups.
Pathological abnormalities of placenta
- Avillous areas (other than those mentioned above):
- Twinning: areas of abutment of the two placentas

 .
. - Endometrial cysts: circular areas 1-3 cm diameter, of little importance.
- Hypoplastic villous areas:
- Pale, thin, shiny plaques in the chorion.
- Small (probably not significant) -> large (significant).
- Old mares with history of endometritis, scarring and cysts.
- Large areas -> fetal growth retardation due to inadequate exchange area.
- Hypoplastic villi may -> poorly developed fetus commonly associated with prolonged gestation (>365 days) and with dysmaturity.
- Mare is high risk in subsequent pregnancies as changes are usually irreversible and inevitably some compromise to fetus.
- Twinning: areas of abutment of the two placentas
- Placental edema:
- In South and South East United States may be related to Fescue grass mycotoxicosis Mycotoxicosis.
- Generalized/local.
- Very significant as indicative of circulatory disorder or inflammation, or both.
- Affects placental transfer both ways.
- Placental hemorrhage/bruising
- Meconium staining:
- Orange-brown tinge to amniotic membranes.
- Indicative of fetal distress.
- Inhalation of meconium is serious.
- Whenever there is meconium staining assume that the neonatal foal is at high risk of sepsis.
- Umbilical cord torsion/displacement:
- Ossification of volk sac remnants:
- The remnants of the embryonic/fetal yolk sac are found in the middle of the allantoic segment of the umbilical cord. They are usually small and liquid-filled, but sometimes ossify, then expand to produce a fluid-filled cavity surrounded by layers of lamellar bone. These pedunculated structures can grow to the size of a football, but are normally much smaller. They rarely cause problems unless they compromise blood flow through the umbilical cord, which can result in abortion.
- Placentitis:
- Affects villous layers of chorion.
- Diffuse or localized.
- Anatomical location of inflammatory responses may correspond to likely portal of entry.
- Chronic changes show significant reduction in efficiency of microvilli → long-term alterations in placental efficiency and compromising development of foal.
- Areas of placentitis are usually paler than the surrounding normal chorion, or tan-brown, and may have exudates on their surface.
- Placentitis in the mare is most commonly ascending, ie infection has tracked up through the cervix and got between the endometrium and the allantochorion.
- Placenta can get infected via systemic (rather than ascending) route.
- Bacterial placentitis
 :
: - Most common type of equine placentitis.
- Specific features recognizable in placentas that have been infected by bacteria.
- 'Dirty' abortion.
- Placental edema and mucopurulent changes over placental surface.
- Cervical/vaginal discharge (before or after parturition).
- Any purulent/fetid vaginal discharge is significant, and if occurring within 12 h of parturition should arouse suspicion of possible sepsis in the foal Foal: neonatal septicemia syndrome.
- Viral placentitis:
- Equine herpes virus 1 (EHV1) (abortion strain) Abortion: EHV-1.
- Occasionally EHV4 involved.
- Respiratory signs in mare in early stages.
- Abortion rapid with early placental separation ('clean abortion').
- Foals born alive are usually weak and non-viable.
- Chorion usually edematous, red and thickened.
- Fungal placentitis:
- Rare.
- Access is usually through the cervix.
- Area of placental star usually affected, occasionally terminal regions of non-pregnant horn.
- Thickened leathery placenta with little/no mucoid/mucopurulent material on surface.
- Most foals born under these circumstances are in an advanced stage of decay at the time of the abortion.
- Placental separation:
- Occurs when the area of the cervical star fails to break during parturition so that the entire allantochorion detaches from the endometrium with the fetus still inside it. 'Red bag' delivery, ie the chorionic side of the allantochorion appears at the vulval lips during foaling. Foal must be extracted as matter of urgency Reproduction: dystocia Umbilical cord: premature separation.
Advantages
- Cheap and easy technique.
- Very informative and must be conducted after parturition.
- Warns of potential problems with foal.
Disadvantages
- Must be performed within 24 h of parturition, unless placenta has been frozen.
Technical problems
- Care must be taken not to spread infectious agents.
Alternative techniques
- Examination of fetus in cases of abortion, but placenta may be of more use and ideally both should be thoroughly examined.
Time required
Preparation
- 10 min.
Procedure
- 30-40 min.
Decision taking
Criteria for choosing test
- Placental examination should be routinely carried out 12-24 h after parturition, or earlier in cases of dystocia/concern about the foal.
Requirements
Subscribe To View
This article is available to subscribers.
Try a free trial today or contact us for more information.
Preparation
Subscribe To View
This article is available to subscribers.
Try a free trial today or contact us for more information.
Technique
Subscribe To View
This article is available to subscribers.
Try a free trial today or contact us for more information.
Aftercare
Subscribe To View
This article is available to subscribers.
Try a free trial today or contact us for more information.
Outcomes
Subscribe To View
This article is available to subscribers.
Try a free trial today or contact us for more information.
Further Reading
Publications
Refereed papers
- Recent references from PubMed and VetMedResource.
- Pozor M (2016) Equine placenta - A clinician's perspective. Part 2: Abnormalities. Equine Vet Educ 28 (7), 396-404 VetMedResource.
- Schlafer D H (2004) Postmortem examination of the equine placenta, fetus and neonate: methods and interpretation of findings. Proc AAEP Congress 144-161 VetMedResource.
- Boosinger T R, Brendemuehl J P, Schumacher J et al (1995) Effects of short-term exposure to and removal from the Fescue endophyte acremonium coenofialium on pregnant mares and foal viability. Biol Reprod, Mono 1, 61-67 Oxford Academic.
- Cross D L, Redmond L M & Strickland J R (1995) Equine fescue toxicosis - signs and solutions. J Anim Sci 73 (3), 899-908 PubMed.
- Collins M H (1993) Placentas and fetal health. Equine Vet J Suppl 4 (14), 8-11 VetMedResource.
- Hong C B et al (1993) Etiology and pathology of equine placentitis. J Vet Diagn Invest 1 (1), 56-63 VetMedResource.
- Cottrill C M et al (1991) The placenta as a determinant of fetal well-being in normal and abnormal equine pregnancies. J Reprod Fertil Suppl 44, 591-601 PubMed.
- Loch W E, Swantner L D & Anderson R R (1987) The effects of four levels of endophyte-infected fescue seed in the diet of pregnant pony mares. J Reprod Fertil Suppl 35, 535-538 PubMed.
- Steven D H et al (1979) Ultrastructural studies of the equine uterus and placenta following parturition. J Reprod Fertil Suppl 27, 579-586 PubMed.
- Whitwell K & Jeffcott L B (1975) Morphological studies on the fetal membranes of the normal singleton foal at term. Res Vet Sci 19, 44-55 PubMed.
Other sources of information
- England G C W (1996) In: Allen's Fertility and Obstetrics in the Horse. 2nd edn. Blackwell Science, USA.